Lung Cancer
Introduction
The rapid pace of lung cancer research continues to give doctors a better understanding of the disease and how to treat it. These advances are offering hope to people with lung cancer and their loved ones. With so much promising information available, it is important to find a lung cancer specialist who can help you make sense of the details about your diagnosis and assist you in making informed treatment decisions.
When you first learn you have cancer, your reactions can range from shock to disbelief, fear to determination. It is important to learn about your diagnosis, listen to the medical team’s advice, ask questions and lean on supportive family and friends.
Diagnostic tests will include blood tests, imaging scans of the chest and brain, a biopsy and molecular testing for biomarkers (see Molecular Testing & Biomarkers).
You may feel that you should start treatment immediately, but in most cases, it is preferable to wait until all of the diagnostic test results are in. Sometimes molecular test results can take up to two weeks. Knowing this ahead of time can help you prepare mentally because it can be stressful to wait. Finding genomic biomarkers through molecular testing, however, is critical in identifying potential therapies. With that information, your doctor can develop the best treatment plan for you based on your cancer’s unique characteristics.
How Lungs Function
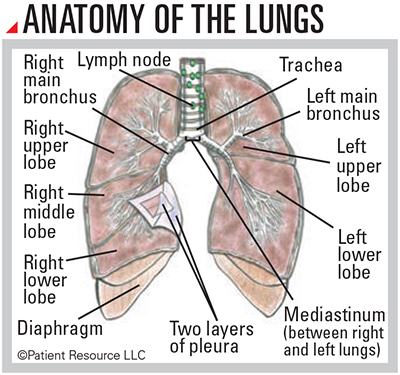
Your lungs are a pair of large, spongy, expandable organs in your chest cavity that are surrounded by a thin layer of protective tissue (pleura). The right lung is a little larger with three parts (lobes), and the left lung has only two (see Anatomy of the Lungs, below).
When you inhale, your lungs absorb oxygen, which is delivered to neighboring red blood cells that then deliver the oxygen to the rest of your body. When you exhale, your lungs rid the body of carbon dioxide. Your diaphragm helps your lungs expand and contract when you breathe.
Cancer develops when abnormal cells in the lining of the airways accumulate to form a tissue mass (primary tumor). A primary tumor may grow into the lining around the lung and form secondary tumors nearby. Many lung cancer patients also have chronic pulmonary disease in the non-cancer tissues of the lung, which may interfere with lung function and alter therapeutic options. Pulmonologists often assist in assessing lung function.
In advanced disease, lung cancer cells break away and enter the bloodstream to form tumors in distant sites such as the opposite lung, liver, brain or bones. These are known as metastases. Even though they are in other parts of the body, they are still considered lung cancer and are treated as such.
Types of Lung Cancer
Pathologic examination of diagnostic biopsies will determine which pathologic type of lung cancer you have: non-small cell lung cancer (NSCLC) or small cell lung cancer (SCLC).
The majority of lung cancer diagnoses are NSCLC, which has several subtypes:
- Adenocarcinoma is the most common NSCLC subtype, especially in people who have never smoked. It generally begins in the mucus-producing cells that are farthest away from the airways. It usually grows more slowly than other types and tends to develop in the peripheral lung and spread to distant sites more often than other types, except for SCLC.
- Squamous cell lung cancer (epidermoid carcinoma) is the second most common subtype. It starts in the early versions of squamous cells, the thin, flat cells that line the inside of the airways in the lungs. It most often develops in the central part of the lung. It spreads to distant sites less often than adenocarcinoma.
- Large cell lung cancer, the least common type of NSCLC, can develop anywhere in the lungs and tends to grow and spread quickly. When large cell lung cancer includes neuroendocrine features, such as higher-than-normal amounts of hormones, it may behave and be treated like SCLC. Other times it may have features more like adenocarcinoma.
SCLC is named for its appearance under a microscope. It often starts in the central airways (bronchi) in the center of the chest. An aggressive form of lung cancer, it most often spreads to distant parts of the body before it is found. Research is underway to explore SCLC subtypes and how they may respond to treatment.
There are other less common types of lung cancer, including mesothelioma, typical and atypical carcinoid tumors, sarcoma and others, which can also begin in other organs.
Seeking a Second Opinion
Getting a second opinion is encouraged for many reasons. It can ensure your diagnosis is accurate by confirming your pathology report and stage of cancer, as well as making you aware of clinical trials to consider.
Doctors bring different training and experience to treatment planning. Some doctors may favor one approach, such as a trial, while others might suggest a different combination of treatments. They can also answer any additional questions you may have.
Most doctors welcome a second opinion and will recommend another physician or hospital. Above all, the goal is for you to have the best care available.