Pain
Neurosurgical options
Neurosurgical options are procedures designed to stop pain at its source by modifying specific brain and spinal cord fibers that carry pain signals. These procedures are performed by a neurosurgeon, a specialist in surgery on the brain and other parts of the nervous system, including the spinal cord, who has expertise in treating pain. Neurosurgical options can include stimulating various components of the nervous system (neurostimulation) and neuroablation, in which the nerve fibers that carry pain are interrupted.
Neurostimulation
Neurostimulation is used most often for pain related to damaged nerves, including treatment-related peripheral neuropathy. This approach can offer important benefits to people with this type of pain, including improved quality of life, the need for less pain medication, the ability to stand or walk for longer periods without pain and the ability to carry out activities that were once painful.
How it works
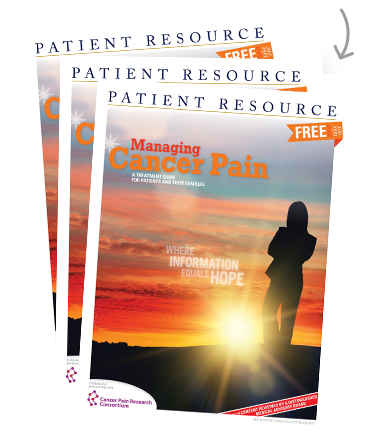
During a neurostimulation procedure, the neurosurgeon implants a small device, about the size of a pacemaker, with a thin wire (known as a “lead”) that is inserted through a needle and placed near the spinal cord (see Figure 1). The device will send low-voltage electricity through the lead to interrupt pain signals before they reach the brain. The pain signal may be replaced with a light tingling sensation that has a soothing feeling over the specific area where pain used to be felt.
How the procedure is done
Because some people are not helped by neurostimulation, the procedure is first done on a temporary basis to make sure that it is a good option. The person lives with the implanted device for about a week; if the device is effective at controlling pain, a “permanent” device is implanted (although it is possible to remove it, if needed).
The procedure is considered to be minor; it is minimally invasive and is usually done on an outpatient basis, which means recovery time is short. The device usually does not interfere with any recreational activities, even swimming. The battery has a long life and will probably not need to be replaced for many years. The device can be turned off or surgically removed if it does not help or if it is no longer needed.
Possible risks
As with all surgical procedures, there are risks associated with a neurostimulation procedure, but most of them are minor. Some of these possible risks include bleeding; infection; and pain, weakness or numbness in the area of the incision site.
Over time, scar tissue may form around the leads or the lead may move, which can affect how the stimulation feels. Also, neurostimulation may be effective initially, but subsequently become less effective after a year or two.
Weighing these potential risks against the possible benefits is important, and you and your doctor will decide if the procedure is the best option for you.
Neuroablation
Neuroablation (or the interruption of nerve fibers carrying pain signals) was once considered to be a last resort for controlling pain because, unlike medications, targeted drug delivery (see here) and neurostimulation, it is irreversible. However, recent medical innovations have opened up many more neuroablation options for relieving pain that can be done at different times during the cancer journey. Thanks to advances in techniques and instruments, these cutting-edge procedures can often be done safely with percutaneous techniques and a local anesthetic, so they are minimally invasive and patients can return to daily activities shortly after the procedure. Even in cases that require open surgical procedure, only a day or two in the hospital may be necessary.
“I’ve had patients fly in from Boston and fly back the next day,” says Dr. William S. Rosenberg, a neurosurgeon in Kansas City, Missouri. “Of all the procedures we do, this type of treatment really suits people who are suffering from pain during their cancer journey. Often, without an incision to heal or a major invasive procedure, we do not have to interrupt chemotherapy or radiation therapy, and excellent pain relief can be achieved while the patient continues those important treatments.”
How it works
Neuroablation procedures work to interrupt certain pain pathways in the brain or spinal cord to achieve pain control. The pathway targeted depends on the type and location of the pain. When you consult with a neurosurgeon with expertise in pain management, he or she will ask you questions about your pain and your overall health to determine if one of these procedures is right for you.
How the procedure is done
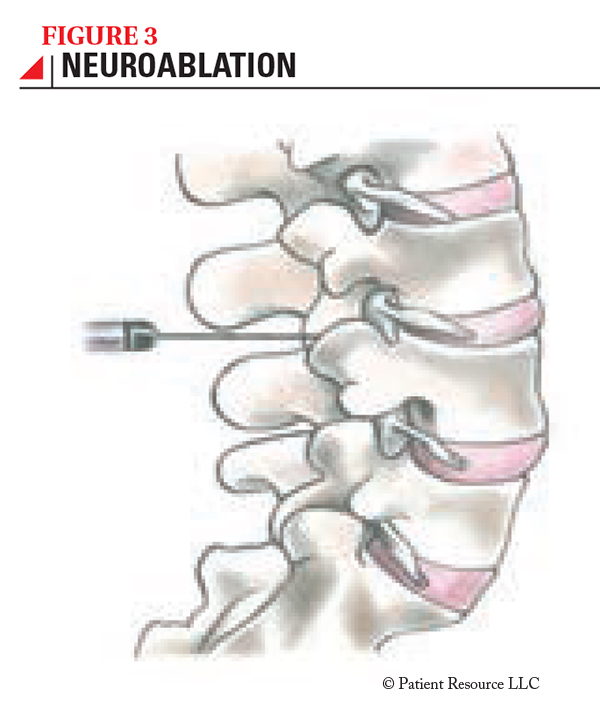
Neuroablation is now primarily done with percutaneous techniques (using a needle through the skin) and imaging (computed tomography, or CT) to help the neurosurgeon identify the precise location of the targeted nerve fibers (see Figure 3). The patient is sedated to be comfortable during the procedure, but is awake so that the neurosurgeon can ask the patient what he or she feels when different areas of the nerve are stimulated. These questions help ensure that the precise nerve fibers are identified. Once the needle is in the right position, a very small electrode is inserted through it and is used to heat the needle tip, which destroys fibers that carry pain signals.
These neuroablation procedures are usually short, sometimes taking only 15 to 30 minutes, and the patient typically requires hospital observation for less than 24 hours. Often the patient can go home the same day. The risk of complications is low. Because the nerve fibers are destroyed, the procedure is permanent. Pain relief is often immediate, although it is possible that it requires some time to take effect. Pain control can range from several months to years or longer, allowing patients to reduce the amount of pain medication they take and to enjoy more activities with a better quality of life.
Cordotomy
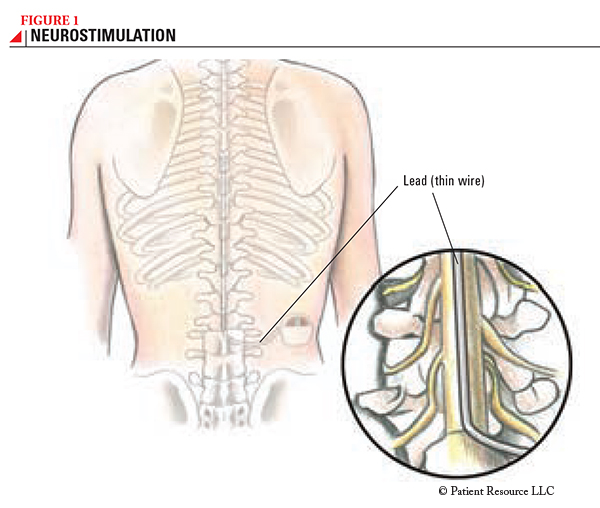
Cordotomy is done to manage pain that is on one side of the body, at or below the shoulder, and the procedure sometimes achieves complete pain relief (see Figure 2). Even if there are other areas of pain, if one of those painful areas is causing a significant problem and is entirely on one side of the body, cordotomy may be considered. Usually, no other function is affected by the procedure, other than perceiving pain (and sometimes hot and cold). On occasion, the patient reports an “odd” sensation in the treated area that is not painful and usually resolves in a few days or weeks. After the procedure, patients can usually go home after a few hours of observation in the hospital.
Myelotomy
Myelotomy is done to disconnect the nerve fibers within the spinal cord that carry pain information from the organs of the abdomen and pelvis, as well as the sacrum (base of the spine). This procedure can be of benefit to people with pain from cancer in the pancreas, liver or ovaries, as well as pain in the rectal, vaginal or perineal area. Side effects are uncommon and can include unsteadiness when walking, urinary retention and leakage of spinal fluid. If these occur, they usually resolve over a few days or weeks.
Radiosurgical hypophysectomy
With radiosurgical hypophysectomy, radiation is used to target the pituitary gland, which is located in the middle of the head, behind the nose. Although the mechanism of action remains unknown, for many years, ablation of the pituitary gland has been effective in relieving pain related to a tumor that has spread (metastasized) to bone. The most common side effects are fatigue for a week or two and, rarely, hormonal changes that can require additional medication. Pain relief has been almost immediate in most patients.