Liver Cancer
Introduction
Living with liver cancer requires strength, and you should not expect to handle it on your own. The good news is you do not have to. The liver cancer community is made up of a variety of experts, organizations and people just like you who are dedicated to helping you live your best life with a liver cancer diagnosis.
Primary liver cancer is a disease in which cancer cells initially form in the tissues of the liver. It is a disease of the hepatobiliary (heh-PAH-toh-BIH-lee-ayr-ee) system. “Hepato” means liver, and “biliary” refers to the gallbladder and bile ducts.
The two main types of primary liver cancer are hepatocellular carcinoma (HCC) and cholangiocarcinoma (also called bile duct cancer). Other types include angiosarcoma, a rare, aggressive form, and hepatoblastoma, the most common type of childhood liver cancer, usually affecting children 3 years or younger. Cancer that begins in other parts of the body and spreads to the liver is not considered liver cancer. Cancer that spreads from elsewhere to the liver is called a metastasis (e.g. colon cancer metastasis).
This guide offers information about HCC, the most common type of liver cancer.
The Role of the Liver
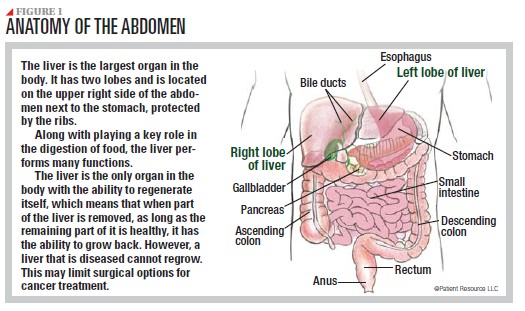
To understand HCC, it helps to know more about your liver:
- It is the largest organ in the body, with two lobes in the upper right side of the abdomen (see Figure 1).
- It performs many functions, including supporting detoxification, digestion, immunity, metabolism, normal blood clotting and vitamin storage.
- It is the only organ in the body that has the ability to regenerate. For example, when part of the liver is removed, it has the ability to grow back — but only if it is healthy.
Learning About HCC
HCC begins in the hepatocellular cells of the liver tissue that are responsible for metabolic functions, detoxification and immune cell activation. Although it can develop in an otherwise healthy liver, it is much more often diagnosed in the presence of an underlying chronic liver condition. That is why it is referred to as “a disease within a disease.”
Several symptoms are associated with HCC, but most patients do not have any symptoms. In some cases of more advanced HCC, one may experience the following:
- Mild to moderate pain or tenderness in the upper right part of the abdomen or right shoulder
- Unintended weight loss
- Abdominal distention
- Deep fatigue
- Vomiting
As HCC becomes advanced and spreads beyond the liver (most commonly to the lung, abdominal lymph nodes or bone), multiple tumors may develop. As a result, you may have these symptoms:
- Ascites (uh-SY-teez), swelling in the abdomen or legs
- Dark urine or light-colored stools
- Jaundice, causing yellow skin and yellowing in the whites of the eyes
Risks and Causes
People often want to know what caused their liver cancer diagnosis. It is not always a single reason. Cirrhosis is the most common underlying chronic condition of HCC. It is a progressive disease that causes inflammation and scarring. Scar tissue causes irreversible damage as it replaces healthy liver cells, causing the liver to gradually lose its ability to function. Cirrhosis itself is not reversible; however, steps can be taken to prevent it from becoming worse (see Table 1). The most common causes of cirrhosis are metabolic dysfunction-associated steatotic liver disease (MASLD), viral hepatitis (hepatitis B or C), and chronic excessive intake of alcohol.
Higher incidence rates of HCC are found in people over 60 and in Asians and Pacific Islanders, African Americans, American Indians/Alaska Natives and Hispanics. Studies attribute this to the fact that some minorities and socioeconomically disadvantaged groups do not have widespread access to surveillance and treatments. Research is also underway to explore other causes, such as higher rates of MASLD, diabetes and other risks. A variety of other factors may increase the risk for HCC. Some are lifestyle-related, but others – your genetic makeup, ethnicity and age – are completely out of your control.
Even though you cannot change certain characteristics about yourself, knowing the factors that may have contributed to your diagnosis can help you process your situation. It can also encourage your loved ones to take steps to reduce the risk factors that they can change (see Table 1).
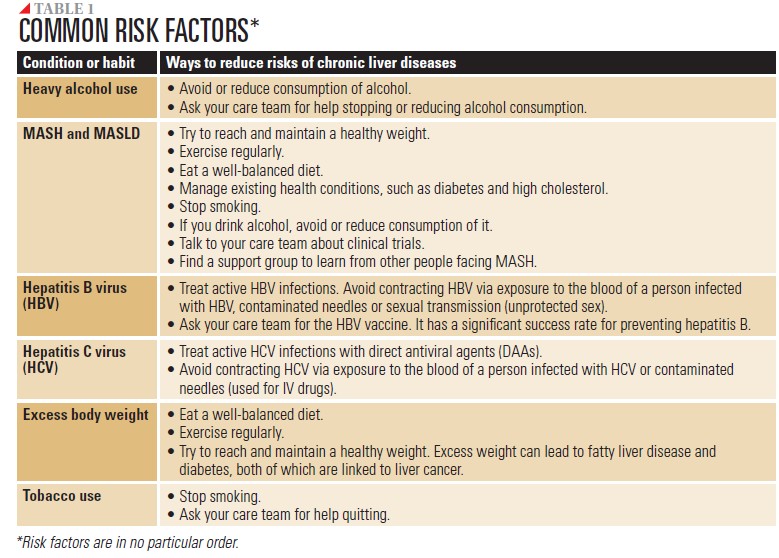
MASLD, formerly known as nonalcoholic fatty liver disease (NAFLD), involves excess fat buildup in the liver. In its most severe form, metabolic-associated steatohepatitis (MASH), formerly known as NASH, can cause cirrhosis, a progressive liver disease that replaces liver cells with scar tissue.
Viral hepatitis B and C, which are carried and spread through contact with blood and other bodily fluids, are also potential underlying conditions.
Your Community Awaits
Get to know the resources around you. They are available as soon as you receive your diagnosis, and they come from multiple areas.
Your multidisciplinary care team involves your doctor and a mix of experienced health and psychosocial care professionals. The specific members of that team will depend on your diagnosis and your needs. They will work with each other and you to plan and manage your treatment. They are also a good resource for a second opinion. You are encouraged to get another opinion from a doctor who has extensive experience treating liver cancer. A second opinion enables you to validate the diagnosis you have been given and hear about other treatment options that may be available.
Case management is a program designed to help manage the practical issues associated with your diagnosis and treatment and reduce your stress and anxiety in the process. If your care team does not have a case mana-ger on staff, ask for a referral.
Palliative care clinicians focus on reducing how aggressively cancer or its treatment causes symptoms or reduces your quality of life.
Advocacy and support groups put you in touch with other people who are familiar with what you are experiencing. Through Blue Faery, the Adrienne Wilson Liver Cancer Association, an advocacy group dedicated to preventing, treating and curing HCC, you will be introduced to programs such as the Liver Cancer Community, Love Your Liver, The Truth about Liver Cancer, and You and Liver Cancer. These programs are designed to give you and your loved ones a forum to learn and discuss the physical and emotional aspects of your diagnosis.
Your community is especially important if you, your loved ones or caregivers face the common issue of disease stigma. Unfortunately, it often goes along with this diagnosis because of the associated underlying conditions of the disease that are sometimes related to lifestyle choices. Do not let negative feelings weigh you down. Adopt a positive mindset and put your energy into managing this diagnosis.



