Advanced Prostate Cancer
Overview
An estimated one out of every seven men in the U.S. will be diagnosed with prostate cancer during his lifetime; in fact, the disease is the most common cancer in men after skin cancer. Advanced prostate cancer – which includes Stages III and IV – is the most aggressive form of the disease. The cancer cells have migrated from the prostate to surrounding tissues and lymph nodes, through the blood and possibly into the bones, tissue and distant organs.
Despite the severity of this disease, however, many treatment options are available for men with advanced prostate cancer that are effective in not only shrinking tumors but also managing treatment-related symptoms and side effects.
This publication will guide you through the basic facts about this disease, along with effective treatment options for you to research and ask your doctors about.
As a patient, you are faced with many important decisions and responsibilities. Educate yourself about all of your options before you commit to a treatment plan, and ask plenty of questions before you decide on the treatment team that will ultimately work with you to manage your health.
About the prostate
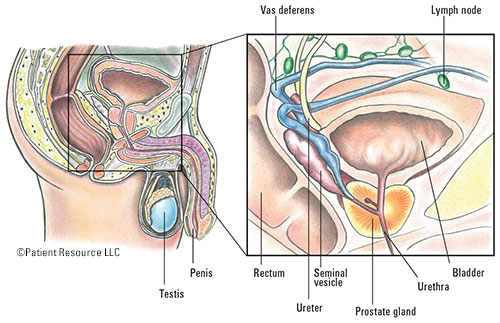
A healthy prostate gland is the size and shape of a walnut, situated under the bladder and in front of the rectum. The prostate wraps around the urethra, which is the tube that carries urine from the bladder and semen from the prostate through the penis (Figure 1).
The main job of the prostate is to produce seminal fluid that protects and transports sperm out of the body. Cancer develops when prostate cells start to mutate into abnormal cells, forming tumors. Some cancer cells slowly and silently spread without causing any symptoms, while others can cause painful symptoms that quickly alert the patient to a problem.
Figure 1
Risk factors
While the actual cause of prostate cancer remains unknown, there are a few risk factors that may increase your chances of developing this disease:
- Age – Men over the age of 65 are the most likely to be diagnosed.
- Race – Not only are African-American men two times more likely to develop this disease than any other race, they are also much more likely to be diagnosed with prostate cancer than any other type of cancer.
- Family history – Your chances significantly increase if close family members were also diagnosed with prostate cancer (especially relatives such as a father, brother or uncle). Changes in the genes inherited from your father or mother also increase the risk of prostate cancer. For example, mutations in the BRCA1 and/or BRCA2 genes, determined through blood testing, can promote cancer growth.
- Veterans – Men who were exposed to Agent Orange (typically Vietnam veterans) are at a higher risk of contracting this disease than those who weren’t. Studies show exposure makes men twice as likely to develop prostate cancer (see At-A-Glance chart).
- Hormones – High levels of testosterone can promote the growth of cancerous cells and may increase the risk of prostate cancer.
- General health – While research is still being conducted to connect a man’s diet with his chances of developing prostate cancer, studies show that men who consume high levels of fat are more likely to be affected by this disease.
Symptoms and side effects
Advanced prostate cancer patients often encounter disease or treatment-related side effects when cancer spreads to other areas of the body. Be aware of your body and ask your doctor how to manage or prevent the following symptoms:
- Pain in hips, thighs or lower back
- Weakened or interrupted urine stream
- Painful or burning urination
- Urgent feeling of having to urinate but not being able to
- Difficulty getting or maintaining an erection
- Blood in the semen or urine
- Shortness of breath, dizziness, paleness
- Unexplained weight loss
- Anemia
- Fatigue
- Bone fractures
Your health care team
The success of your treatment depends on several factors, including the expertise of the specialists you choose to care for you. Do plenty of research and question your potential treatment team about their abilities and experience treating your specific type and stage of cancer. As with all important decisions, you should also pay close attention to your instincts and trust your gut before committing to any type of treatment.
Also, don’t be shy about getting a second opinion. Choosing the right treatment and selecting the right people to be in your corner during this time is crucial and is one of your biggest responsibilities as a patient. Here are a few of the different types of doctors you’ll likely encounter during your treatment and recovery:
- Urologist – A physician trained to treat the male reproductive system and problems related to the urinary tract (kidneys, ureters, bladder, prostate and urethra).
- Urologic oncologist – A specialized surgeon who treats cancer of the urinary tract and reproductive system.
- Radiation oncologist – A physician who uses radiation to treat cancer and manages side effects of your treatment.
- Medical oncologist – A physician who treats cancer with chemotherapy and hormone therapy and manages general problems that arise. Some medical oncologists specialize in treating patients with urinary and male reproductive tract cancers.
Once treatment begins, it will be very important to keep everyone on your team posted about any symptoms or side effects you encounter so that they can be managed to make you more comfortable and keep you on schedule. It can be hard to strike a balance between effective disease control and living with the side effects, but your treatment team can help you find that balance.
While you’re undergoing treatment, you will have frequent follow-up visits with your doctors to make sure the disease is responding to your treatment and to evaluate your progress. These are two very important factors when it comes to deciding whether to continue with your current treatment or switch to something else that might be more effective.
You may find it helpful to keep a journal of how you’re feeling on a daily/weekly basis so that you can relay any changes or concerns you experience to your treatment team.