HER2- Advanced Breast Cancer
Treatment Planning
When breast cancer is or becomes metastatic, the treatment plan shifts from cure to management, which means preventing or slowing the spread of the cancer and relieving any pain or discomfort. Do not, however, let that distress you. New treatment strategies and ongoing research are offering many people more hope for longer, fuller lives. The goal of reaching “no evidence of disease” may be a very real possibility.
Discuss your goals of treatment. A key part of that is how you hope your daily life will look. Start with questions like these:
- Where will I get my treatments? Are any of them oral so I can take them at home?
- What side effects should I expect, and what is the plan for preventing or managing them?
- When should I begin palliative care?
- Can we adjust treatment times around my work schedule?
- If my cancer becomes resistant, will I have other options? This is also a good time to have an honest conversation about when and why to make the difficult decision of whether to stop treatment.
Drug Therapy
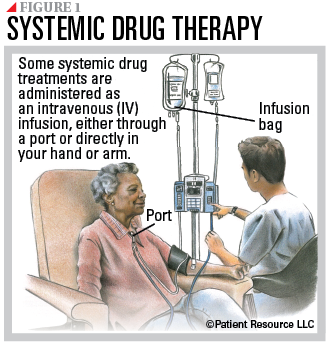
Many drug therapies, including targeted therapy, hormone therapy, chemotherapy and immunotherapy, have been developed to treat different combinations of ER, PR and HER2 receptor expression (see Table 1). Often these drugs are used in combination, and it is common for more than one therapy to be included in your treatment plan. These treatments are systemic because they travel throughout the body. You may receive them through an IV into a vein, through a port in your body, as an injection (shot) or orally as a pill or liquid (see Figure 1).
Targeted therapy uses drugs or other substances to identify, attack and destroy specific types of cancer cells or to slow disease progression. Some interfere with the cancer cells’ internal functions; others attack specific receptors on the cancer cells’ surfaces; and some target the blood vessels that supply the tumor. More recently, targeted therapy was approved to be used alone to treat metastatic HER2-low breast cancers, which may include some diagnoses of triple negative breast cancer (TNBC). Other targeted therapy drugs are sometimes used in combination with hormone therapy to treat ER+ or PR+ breast cancers or HER2- breast cancer with the BReast CAncer 1 or 2 (BRCA1 or BRCA2) gene mutations.
These types of targeted therapy may be used:
- Anti-HER2 antibody drugs are laboratory-made proteins that can bind to cancer cells and target the HER2 receptor. They can be used alone or to carry drugs, toxins or radioactive substances directly to cancer cells. This type may be used for HER2-low breast cancer.
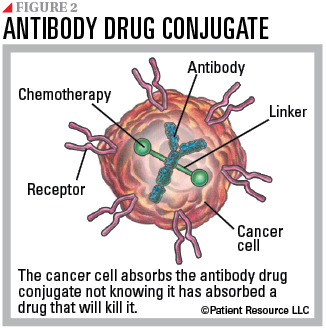
- Monoclonal antibodies (mAbs) are commonly used. Laboratory-made mAbs that are combined with a toxin such as a chemotherapy drug are known as antibody drug conjugates. Recently approved to treat the newly designated HER2-low breast cancer subtype, a mAb attaches to the HER2 receptor on a cancer cell, gets swallowed by the tumor cell and breaks down inside the cell, releasing the chemotherapy drug, preventing growth signals from HER2 receptors and causing cell death (see Figure 2).
- Kinase inhibitors target cancer cells’ ability to grow and survive by targeting kinases, which are enzymes that speed up chemical reactions in the body. These inhibitors can be designed to attack enzymes within a cell, proteins or enzymes needed for a cell’s growth, or receptors on the cell’s surface. Therapies targeting the NTRK gene fusion may also be used. This fusion occurs when a piece of the chromosome containing a gene called NTRK breaks off and joins with a gene on another chromosome.
- A PIK3CA inhibitor prevents the growth of cells by blocking the PIK3CA gene, which is frequently mutated in breast cancer.
- Poly (ADP-ribose) polymerase (PARP) inhibitors prevent cancer cells from repairing themselves and lead to tumor cell destruction.
- Tumor-agnostic treatment targets specific genetic mutations to prevent growth regardless of cancer type or where it is.
Hormone therapy, also called endocrine therapy, is primarily used to treat cancer that is estrogen- and/or progesterone-receptor positive (ER+/PR+). It is actually an anti-hormone because it reduces or blocks the stimulating effect of the hormones on tumor cells. When tumor cells test positive for one or both hormone receptors (ER+ and/or PR+), it means hormones are fueling the cancer’s growth. Blocking hormone receptors or blocking production of hormones by the body can be highly effective in slowing cancer growth or stopping progression.
Hormone therapy is not effective for cancer that is ER-/PR- because the growth is not driven by hormones. In some cases, biopsied tumor cells may test negative for all three biomarkers (ER-, PR-, HER2-), which is referred to as TNBC.
Depending on your past and current treatments, the length of time before recurrence, how far the cancer has spread, gender and menopausal status (for women), your treatment plan may include any of the following:
- Anti-estrogens are substances that keep cells from making or using estrogen. They may stop some cancer cells from growing or even destroy them.
- Aromatase inhibitors are drugs that prevent the production of estrogen, a female hormone, by interfering with an aromatase enzyme. They may benefit postmenopausal women with hormone-dependent breast cancer or younger women whose ovarian function is blocked by drugs or who have had their ovaries removed. Aromatase inhibitors cannot be used in premenopausal women with functioning ovaries.
- Very high doses of hormones may be used to stop cancer growth.
- Ovarian ablation uses surgery, radiation or extreme heat or cold to permanently stop the ovaries from making hormones.
- Ovarian suppression can stop the ovaries from making hormones that promote cancer growth in ER+/PR+ cancers. Drugs called luteinizing hormone releasing hormone (LHRH) agonists are typically used instead. For premenopausal women, these drugs provide an equivalent alternative to removing the ovaries. Selective estrogen receptor downregulators (SERDs) are also a form of ovarian suppression that block estrogen from attaching to the hormone receptors on the tumor.
- Bilateral oophorectomy is surgery to remove both ovaries. It may be an ablation option for some premenopausal women.
Immunotherapy harnesses the potential of the body’s own immune system to recognize and destroy cancer cells. Various types of immunotherapy are approved for advanced and metastatic breast cancer.
- Immune checkpoint inhibitors prevent the immune system from slowing down, allowing it to keep up its fight against the cancer. These drugs do this by targeting and blocking PD-1 or PD-L1.
- Tumor-agnostic treatment, when used as immunotherapy, is approved to treat any type of cancer that has molecular alterations known as microsatellite instability-high (MSI-H), deficient mismatch repair (dMMR) or tumor mutational burden-high (TMB-H).
Chemotherapy kills rapidly multiplying cells throughout the body. It can be given as a single drug or usually is combined with other chemotherapy drugs or other types of treatment. It is most often used to treat ER-/PR- cancers or ER+/PR+ cancers that no longer respond to hormone therapy.
It may be used for metastatic TNBC that does not express PD-L1 and for metastatic ER+, PR+, HER2- or HER2-low breast cancer when hormonal therapy is not effective.
Bone-strengthening drugs or bone-modifying agents may be used in addition to systemic treatment or radiation therapy to prevent or delay bone fractures when breast cancer has spread to the bones.
TABLE 1. RECEPTOR AND TREATMENT RESPONSE
| Receptors | Likely Treatment Response |
| ER+ and/or PR+, HER2+ (triple positive) | Typically responds to anti-estrogen drugs (hormone therapy) and anti-HER2 drugs (targeted therapy) |
| ER- and PR-, HER2+ | Typically responds to anti-HER2 drugs (targeted therapy) and to chemotherapy but not to anti-estrogen drugs (hormone therapy) |
| ER+ and/or PR+, HER2v- | Typically responds to anti-estrogen drugs (hormone therapy), but not likely to respond to anti-HER2 drugs |
| ER+ and/or PR +, HER2-low | Typically responds to anti-estrogen drugs and anti-HER2 drugs |
| ERR- and PR-, HER2- (triple negative) | Typically treated with chemotherapy and immunotherapy; not likely to respond to anti-estrogen drugs (hormone therapy) or anti-HER2 drugs |
| ER- and PR-, HER2-low | Typically treated with chemotherapy, may be treated with anti-HER2 drugs (targeted therapy) and immunotherapy; not likely to respond to anti-estrogen drugs (hormone therapy) |
Radiation Therapy
This therapy uses high-energy X-rays to kill cancer cells or keep them from growing. Sometimes it is given to control symptoms caused by breast cancer that has spread to specific organs, such as the bones or the brain. It may be used for pain management or to reduce the size of tumors causing discomfort.
Surgery
Though not a primary treatment, surgery may be an option to alleviate pain related to large tumors or metastases in the brain, spine or lungs, or to help support or stabilize weakened or broken bones.
Clinical Trials
These medical research studies, which offer access to therapies not yet widely available, may become part of your treatment plan. The advances from clinical trials, including the new HER2-low distinction and treatment with an antibody drug conjugate, are offering more hope for the breast cancer community.
Ongoing Monitoring & Communication
Your doctor will monitor you closely with tests and imaging so that your treatment plan can be adapted as needed, making it important to stay on schedule with follow-up appointments.
|
Commonly Drug Therapies for Advanced Breast Cancer
These therapies may be used alone or in combination. |
| Targeted Therapy |
| abemaciclib (Verzenio) |
| alpelisib (Piqray) |
| entrectinib (Rozlytrek) |
| everolimus (Afinitor, Afinitor Disperz) |
| fam-trastuzumab deruxtecan-nxki (Enhertu) |
| larotrectinib (Vitrakvi) |
| olaparib (Lynparza) |
| palbociclib (Ibrance) |
| ribociclib (Kisqali) |
| ribociclib and letrozole (Kisqali Femara Co-Pack) |
| ribociclib (Kisqali) |
| sacituzumab govitecan-hziy (Trodelvy) |
| talazoparib (Talzenna) |
| Hormone Therapy |
| anastrozole (Arimidex) |
| elacestrant (Orserdu) |
| ethinyl estradiol |
| exemestane (Aromasin) |
| fluoxymesterone |
| fulvestrant (Faslodex) |
| goserelin acetate (Zoladex) |
| letrozole (Femara) |
| leuprolide acetate (Eligard, Lupron, Lupron Depot) |
| megestrol acetate (Megace) |
| tamoxifen |
| toremifene (Fareston) |
| Immunotherapy |
| dostarlimab-gxly (Jemperli) |
| pembrolizumab (Keytruda) |
| Chemotherapy |
| capecitabine (Xeloda) |
| carboplatin (Paraplatin) |
| cisplatin |
| cyclophosphamide |
| docetaxel (Taxotere) |
| doxorubicin (Adriamycin) |
| epirubicin (Ellence) |
| eribulin (Halaven) |
| fluorouracil (5-FU) |
| gemcitabine (Gemzar) |
| ixabepilone (Ixempra) |
| liposomal doxorubicin (Doxil) |
| paclitaxel (Taxol) |
| protein-bound paclitaxel (Abraxane) |
| vinorelbine (Navelbine) |