Liver Cancer
Treatment Planning
Progressive research in treatment is enabling some people with HCC to manage their illness as they would other chronic conditions. And for others, the advances may even mean a cure. As you learn more about your diagnosis and treatment options, you are encouraged to participate in shared decision making with your medical team. Always ask questions and share your expectations about your quality of life. Being informed will help you feel more comfortable moving forward.
To develop the most effective treatment plan, your doctor will coordinate with your medical team. Together, you will create a treatment plan that is based on the following:
- The results of a thorough health assessment, diagnostic tests and imaging
- How much of your liver is affected by the tumor
- The number of tumors, including their size and location
- Whether the cancer has spread outside the liver
- How well your liver is working and whether noncancerous areas remain healthy
- Any comorbidities (other serious health conditions)
- Your overall physical condition
- Your preferences about quality of life
Your prognosis (outlook) will help guide your goals of treatment. Those goals may be as follows and may change over time:
- Eliminating the HCC by curing it; also referred to as a curative treatment
- Shrinking the tumor(s) to make liver resection or transplantation possible; also referred to as downsizing the tumor
- Slowing the cancer’s progression to extend life
- Using supportive (palliative) care to improve your quality of life by managing side effects, treating post-operative pain and symptoms, or helping relieve pain and discomfort without active treatment
Common HCC Treatments
One or more of these options may be part of your treatment plan.
Surveillance (also called watchful waiting) may be recommended for tumors that appear to be growing very slowly. With close monitoring and regularly scheduled blood and imaging tests (every 3 months is common), this allows you to avoid potential side effects for as long as possible before treatment is necessary. Make and keep these appointments because treatment should begin if the pace of cancer progression increases.
Clinical trials are a valuable option, especially if you are diagnosed with advanced HCC. Ask your doctor whether you should consider a clinical trial immediately after diagnosis or at any other time during your treatment (see Clinical Trials).
Surgery is the primary curative method for treating HCC. It is often complex and requires a high degree of training and skill. It is recommended that you seek treatment at a cancer facility known for performing a high volume of liver surgical procedures, and one that has liver transplant as an option. Seek a second or third opinion before deciding on a surgeon.
Liver resection, also called a partial hepatectomy (HEH-puh-TEK-toh-mee), removes a wedge, an entire lobe or more of the liver that contains the tumor(s), along with a margin of healthy tissue. The remaining healthy liver will continue to function as it regenerates (regrows), often to near normal size. This may be an option when your liver is functioning well, the tumors are small, the disease is early-stage and blood vessels are not involved. You and your liver must be healthy enough to have surgery.
- Traditional open resection is used for complex operations. The surgeon makes an incision into the abdomen. This is major surgery and requires significant recovery time.
- Minimally invasive laparoscopic surgery may be an option for resections, depending on the tumor location and surgeon experience. A few small incisions are made in the abdomen to insert a long, tube-like medical instrument (laparoscope) with a tiny video camera on the end. Magnified images from inside the body are transmitted to a video screen in the operating room to guide the surgeon. The surgeon still typically needs to make one larger incision to remove the tumor from your abdomen. Nevertheless, this method usually results in shorter recovery time and fewer complications than traditional open resection.
Liver transplantation is a highly effective, potentially curative treatment for HCC. The entire liver is removed (hepatectomy) and replaced with a healthy liver, most often from a deceased donor. In some cases, a living donor may be used.
Only a very small percentage of people qualify for transplantation. Candidates must meet strict criteria concerning the size, stage, location and number of tumors present, and must have a qualifying “liver score” based on blood levels of creatinine, bilirubin, sodium and blood clotting factors. It is beneficial to have your evaluation in a center that performs liver transplants. If your doctors believe you may be a candidate, you can be referred for assessment to a transplant team.
If you are a candidate, you will likely undergo bridging treatment while you wait for a liver to become available. This is necessary because the wait time can be significant in some cases. Bridging therapy is designed to prevent the cancer from growing or spreading during the wait. Bridging treatments may include ablation, embolization, radiation therapy or systemic drug therapy.
Radiofrequency ablation (RFA) therapy may be a curative option for HCC when a tumor is unresectable (inoperable) or surgery is not an option for another reason. It is a minimally invasive, image-guided procedure that kills cancer cells. A needle is inserted through the skin directly into the tumor and an electrical current is run through it to subject the tumor to extreme temperatures. Other ablation therapies include the following:
- Microwave ablation (MWA) uses microwave energy.
- Cryoablation, also called cryosurgery or cryotherapy, delivers extremely cold gas through a hollow needle. This may be referred to as thermal ablation.
- Percutaneous ethanol injection (PEI), also called alcohol ablation, delivers ethanol (alcohol) directly into the tumor.
Embolization procedures are not curative but can be very effective in extending life and improving quality of life:
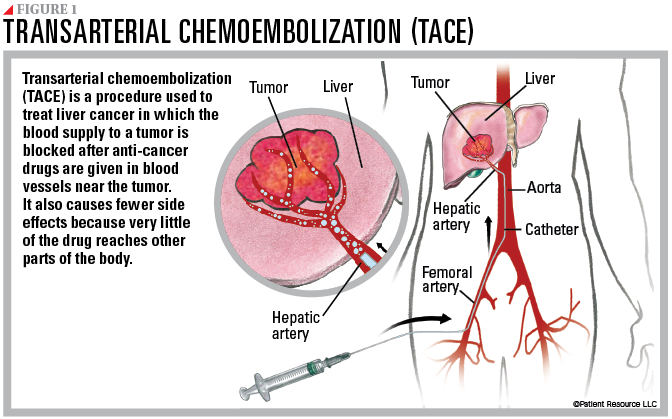
Transarterial chemoembolization (TACE) involves making a small incision in the groin and inserting a catheter, which is a thin, flexible tube that is guided through the body to the hepatic artery. It is a minimally invasive, image-guided procedure that treats HCC by administering chemotherapy into small hepatic arteries that are the main source of blood for most tumors developing in the liver, and then blocking them off to allow the chemotherapy to remain present in the area of the tumor for longer periods of time (see Figure 1). Very little of the chemotherapy escapes the liver, making conventional side effects from chemotherapy uncommon.
Transarterial bland embolization (TAE) is a similar procedure. When the catheter is in place, tiny particles made of gelatin beads or sponges are injected to block small arteries, cutting off the flow of blood feeding the tumor (without administration of chemotherapy). Healthy liver tissue continues to receive blood from other blood vessels.
Radioembolization, also referred to as Y90 or Yttrium 90, combines radiation therapy with embolization. Microscopic glass beads containing high-dose radiation are injected into the hepatic artery to be delivered directly to the tumor. The radiation kills many cancer cells. The goal is to slow the growth of the tumors and reduce symptoms, although radioembolization has also been used to reduce the size of tumors to permit subsequent surgical treatment.
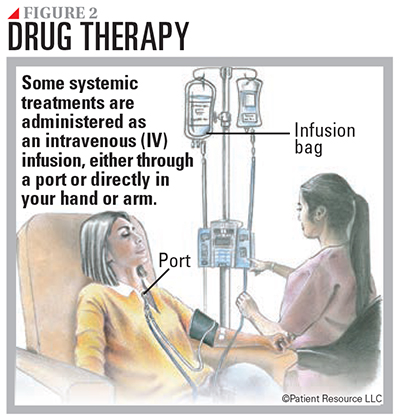
Drug therapy may be used to manage HCC. It is systemic therapy, which means the drugs travel throughout the body (see Figure 2).
Molecularly targeted therapy is designed to slow the cancer’s progression. Drugs travel through the bloodstream looking for specific proteins and tissue environments to block cancer cell signals and thereby restrict the growth and spread of cancer. The most commonly used for HCC is an angiogenesis inhibitor. It works by blocking the growth of new blood vessels that feed the cancer cells. Blood vessels deliver nutrients the tumors need to grow and spread, so by shutting down the formation of new blood vessels, angiogenesis inhibitors in effect “starve” the tumor. Other targeted therapies treat mutations in the neurotrophic tyrosine receptor kinase (NTRK) (pronounced EN-track) gene, which causes cancer cells to grow. Many targeted therapies are taken orally at home. Targeted therapy may be used alone or in combination with immunotherapy.
Immunotherapy fights cancer by stimulating the body’s immune system to recognize and destroy cancer cells. Immune checkpoint inhibitors are the type of immunotherapy currently approved to be used for advanced HCC in certain instances. These drugs prevent the immune system from slowing down, allowing it to keep up its fight against the cancer. The following checkpoint receptors are targets for immunotherapy:
- PD-1 (programmed cell death protein 1) is a receptor involved with signaling T-cells to die and reducing the death of regulatory T-cells (suppressor T-cells). PD-1 can signal the immune system to slow down only if it connects with PD-L1.
- PD-L1 (programmed death-ligand 1) is a protein that, when combined with PD-1, sends a signal to reduce the production of T-cells and enable more T-cells to die. When PD-1 (the receptor) and PD-L1 (the protein) combine, the reaction signals that it is time to slow down.
- CTLA-4 (cytotoxic T-lymphocyte-associated protein 4) is another checkpoint like PD-1. CTLA-4, however, can connect with more than one protein.
This type of immunotherapy is given intravenously (IV). It may be used alone or combined with another immunotherapy or targeted therapy.
Radiation therapy uses high-energy X-rays or other types of radiation to destroy cancer cells. The goal is to shrink tumors or slow their growth. It may be used in palliative care to relieve pain and other cancer symptoms by shrinking tumors. It is sometimes referred to as stereotactic body radiotherapy (SBRT).
| Drug Therapies for HCC |
| cabozantinib (Cabometyx) |
| entrectinib (Rozlytrek) |
| larotrectinib (Vitrakvi) |
| lenvatinib (Lenvima) |
| pembrolizumab (Keytruda) |
| ramucirumab (Cyramza) |
| regorafenib (Stivarga) |
| sorafenib (Nexavar) |
| Possible Combination Therapies |
| atezolizumab (Tecentriq) with bevacizumab (Avastin) |
| ipilimumab (Yervoy) and nivolumab (Opdivo) |
| tremelimumab (Imjudo) with durvalumab (Imfinzi) |


