Head & Neck
Laryngeal Cancer
Includes illustrated staging details
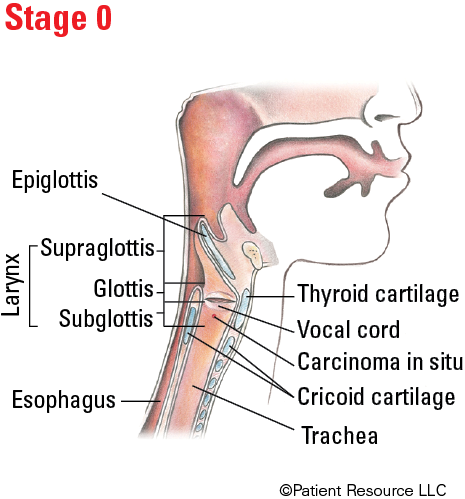
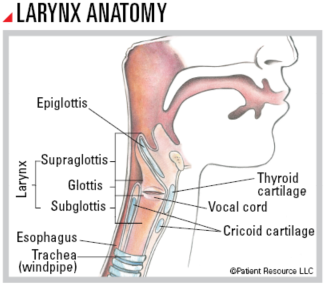
Often called the voice box, the larynx (LAYR-inx) is a short, hollow organ in the lower part of your throat that contains the vocal cords. It is part of the respiratory system and is a passageway to the lungs that is involved in your ability to talk, breathe and swallow. Cartilage walls that form your Adam’s apple protect the vocal cords. When you swallow, a tissue flap called the epiglottis (eh-pih-GLAH-tis) covers your trachea (windpipe) to keep food and liquid from entering your lungs.
The larynx, which is only two inches long, has three parts. The vocal cords are in the middle part called the glottis. Above is the supraglottis, and below is the subglottis, which ends at the top of your trachea.
Called laryngeal (layr-en-JEE-ul) cancer, cancer of the larynx most often first develops in the organ’s moist lining in thin, flat squamous (SKWAY-mus) cells and is called squamous cell carcinoma.
Your doctor will evaluate your voice, breathing and swallowing functions before treatment begins. You will also discuss the benefits and risks of each treatment option and the impact potential side effects and late effects may have on your quality of life.
Treatment Options
The primary goal of your health care team will be to focus on preserving (as much as possible) your larynx because removing, destroying or shrinking the tumor will affect your ability to speak, eat and breathe.
One or more of the following treatments may be used.
Surgery is a common treatment for early glottic cancers and locally advanced T4a tumors. It is less common to treat T2 to T3 tumors surgically. The following procedures, beginning with least invasive, may be recommended.
Vocal cord stripping removes the superficial layers of tissue on the vocal cords. This technique can be done for a biopsy sample or to treat pre-cancers and early-stage cancers of the vocal cords. Most people can eat, speak and breathe normally after recovery.
Endoscopic resection is performed through an endoscope (a thin, lighted camera) and is used to remove cancer that is confined to the vocal cords or is early stage.
Transoral laser microsurgery (TLM) avoids the need for neck incisions and may be used to remove laryngeal cancers that are superficial or limited in extent.
Cordectomy removes all or part of a vocal cord and may be used to remove small cancers of the glottis. Removing part of a vocal cord typically causes permanent hoarseness and may cause temporary swallowing difficulties.
Laryngectomy removes all or part of the larynx. Your ability to speak after recovering from surgery depends on how much of the larynx is removed:
- Supraglottic laryngectomy removes the part of the larynx above the vocal cords and may be used when tumors are confined to the supraglottis. Speech therapy will be necessary after recovery, and the effect on speech varies.
- Vertical hemilaryngectomy may be used to treat cancers of the vocal cords. It involves removing one vocal cord and leaving the other intact. You may still have some ability to speak, but your speech will change.
- Supracricoid laryngectomy removes a large part of the larynx, including both vocal cords. Your ability to speak is preserved, although how you speak will change.
Because all of the above types of laryngectomy also affect your ability to safely swallow, most patients require at least a temporary feeding tube during recovery. Many patients will also need a tracheostomy tube after surgery that may be removed once everything is healed and the swelling has resolved. Patients with underlying lung problems, such as COPD or emphysema, are generally not candidates for this type of surgery.
Total laryngectomy removes the entire larynx and vocal cords. This surgery permanently separates the trachea (windpipe) from the esophagus and then attaches the trachea to a hole created in the front of the neck called a stoma. The stoma is the new airway to breathe through instead of breathing through your mouth and nose. A total laryngectomy may be used to treat advanced or recurrent cancers when there are no other viable options. Following recovery, you must learn new ways to communicate because normal speech is no longer possible. Most of the time, you will be able to swallow after you heal from surgery. If your doctor performs a laryngectomy, you may also have reconstructive surgery (see Reconstruction & Rehabilitation).
A neck dissection to remove some lymph nodes in your neck may be recommended. Your doctor will consider the exact location and stage of your tumor.
Radiation therapy with or without chemotherapy is an option for many patients and is often called organ preservation treatment — meaning you keep your larynx. Radiation is typically an option for patients with T1 to T3 tumors. Radiation may also be used for patients with more advanced tumors that are not candidates for surgery.
If radiation therapy is a part of your treatment plan, it is recommended you have a pre-treatment evaluation by an oncologic dentist and speech pathologist before receiving radiation therapy (see Dental & Oral Side Effects). Smoking can interfere with the effectiveness of this treatment, so it is recommended that you stop before beginning therapy.
External-beam radiation therapy (EBRT) is most commonly used to treat laryngeal cancer. It is typically given once daily for a set amount of time. Types of EBRT include three-dimensional conformal radiation therapy (3D-CRT) and intensity-modulated radiation therapy (IMRT).
Another type, hyperfractionated radiation therapy, involves treatments containing small doses of radiation given more than once a day. It is given over the same period of time as standard radiation therapy.
Chemoradiation therapy combines radiation therapy with chemotherapy for more advanced cancers. They are frequently used together because chemotherapy often enhances the effectiveness of radiation therapy. It may be used if organ preservation surgery is not an option.
For advanced stage cancers, radiation with or without chemotherapy may be recommended to eliminate any remaining cancer cells and to lower the risk of recurrence.
Drug therapy may be used alone or in combination with other therapies.
Chemotherapy may be used alone, or before surgery or radiation therapy, or both. Chemoradiation therapy may be used after surgery to decrease the likelihood of recurrence. It may be the primary treatment in some cases. If no traces of the tumor remain, surgery may not be necessary.
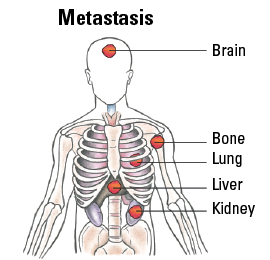
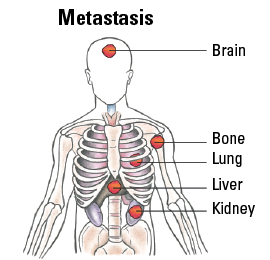
Immunotherapy in the form of immune checkpoint inhibitors may be used to treat recurrent or metastatic laryngeal cancer if surgery or chemoradiation is not an option. The doctor will test for the tumor’s PD-L1 expression, which may indicate whether the tumor could respond to immunotherapy. If expression is more than 1 percent, the tumor is considered to be PD-L1 positive, and immunotherapy alone may be used. If PD-L1 is negative, immunotherapy and traditional chemotherapy are often combined for recurrent or metastatic cancer.
Targeted therapy may be used for laryngeal cancer that contains specific genetic abnormalities, proteins or growth factors. Epidermal growth factor receptor (EFGR) inhibitors are approved in combination with radiation therapy for laryngeal cancer that has not spread. EGFR inhibitors may be used with chemotherapy for metastatic laryngeal cancer.
TNM Classification for Laryngeal Cancer
| Classification | Definition |
| Tumor (T) | |
| TX | Primary tumor cannot be assessed. |
| Tis | Carcinoma in situ. |
| Supraglottis | |
| T1 | Tumor limited to one subsite of supraglottis with normal vocal cord mobility. |
| T2 | Tumor invades mucosa of more than one adjacent subsite of supraglottis or glottis or region outside the supraglottis (e.g., mucosa of base of tongue, vallecula, medial wall of pyriform sinus) without fixation of the larynx. |
| T3 | Tumor limited to larynx with vocal cord fixation and/or invades any of the following: postcricoid area, preepiglottic space, paraglottic space, and/or inner cortex of thyroid cartilage. |
| T4 | Moderately advanced or very advanced. |
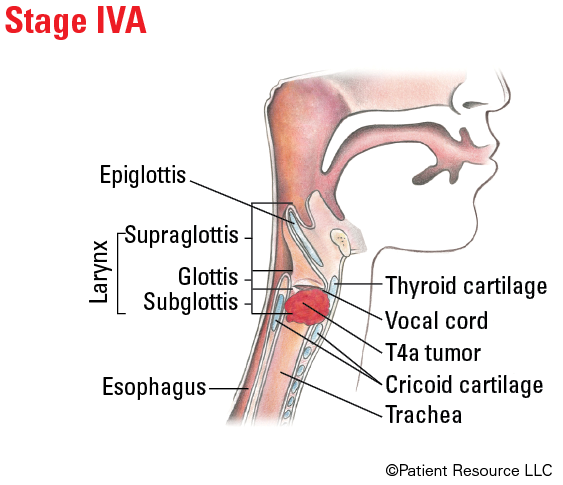
| T4a | Moderately advanced local disease. Tumor invades through the outer cortex of the thyroid cartilage and/or invades tissues beyond the larynx (e.g., trachea, soft tissues of neck including deep extrinsic muscle of the tongue, strap muscles, thyroid or esophagus). |
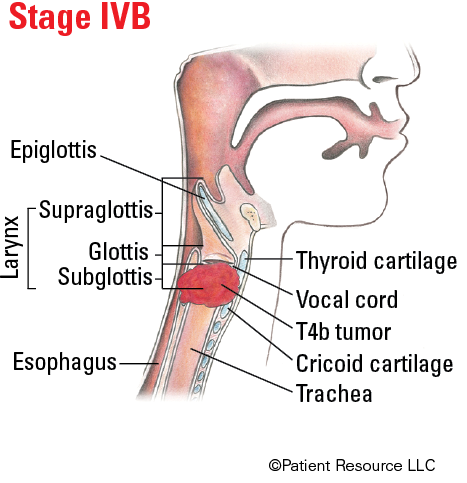
| T4b | Very advanced local disease. Tumor invades prevertebral space, encases carotid artery, or invades mediastinal structures. |
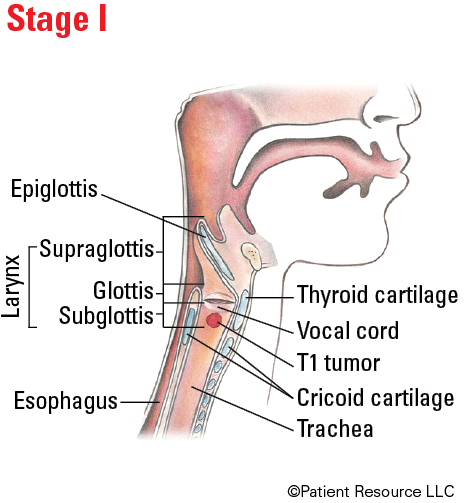
| Glottis | |
| T1 | Tumor limited to the vocal cord(s) (may involve anterior or posterior commissure) with normal mobility. |
| T1a | Tumor limited to one vocal cord. |
| T1b | Tumor involves both vocal cords. |
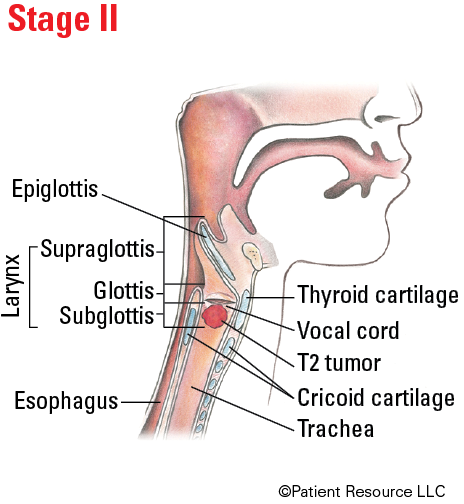
| T2 | Tumor extends to supraglottis and/or subglottis, and/or with impaired vocal cord mobility. |
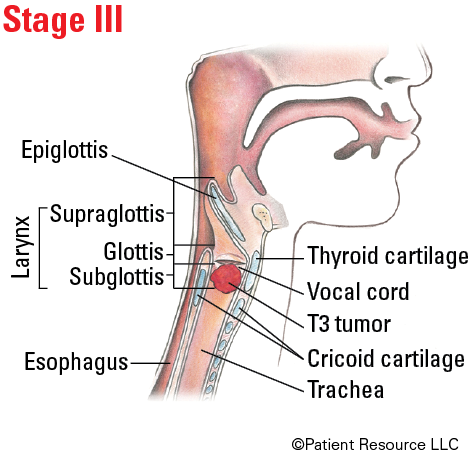
| T3 | Tumor limited to the larynx with vocal cord fixation and/or invasion of paraglottic space and/or inner cortex of the thyroid cartilage. |
| T4 | Moderately advanced or very advanced. |
| T4a | Moderately advanced local disease. Tumor invades through the outer cortex of the thyroid cartilage and/or invades tissues beyond the larynx (e.g., trachea, cricoid cartilage, soft tissues of neck including deep extrinsic muscle of the tongue, strap muscles, thyroid or esophagus). |
| T4b | Very advanced local disease. Tumor invades prevertebral space, encases carotid artery or invades mediastinal structures. |
| Subglottis | |
| T1 | Tumor limited to the subglottis. |
| T2 | Tumor extends to vocal cord(s) with normal or impaired mobility. |
| T3 | Tumor limited to larynx with vocal cord fixation and/or invasion of paraglottic space and/or inner cortex of the thyroid cartilage. |
| T4 | Moderately advanced or very advanced. |
| T4a | Moderately advanced local disease. Tumor invades cricoid or thyroid cartilage and/or invades tissues beyond the larynx (e.g., trachea, soft tissues of neck including deep extrinsic muscles of the tongue, strap muscles, thyroid, or esophagus). |
| T4b | Very advanced local disease. Tumor invades prevertebral space, encases carotid artery or invades mediastinal structures. |
| Node (N) | |
| NX | Regional lymph nodes cannot be assessed. |
| N0 | No regional lymph node metastasis. |
| N1 | Metastasis in a single ipsilateral (on the same side) lymph node, 3 cm or smaller in greatest dimension and ENE*(-). |
| N2 |
Metastasis in a single ipsilateral (on the same side) lymph node, 3 cm or smaller in greatest dimension and ENE*(+);
or larger than 3 cm but not larger than 6 cm in greatest dimension and ENE(-); or metastases in multiple ipsilateral lymph nodes, none larger than 6 cm in greatest dimension and ENE(-); or in bilateral (on both sides) or contralateral (on the opposite side) lymph node(s), none larger than 6 cm in greatest dimension and ENE(-). |
| N2a |
Metastasis in single ipsilateral (on the same side) node, 3 cm or smaller in greatest dimension and ENE*(+);
or a single ipsilateral node, larger than 3 cm but not larger than 6 cm in greatest dimension and ENE(-). |
| N2b | Metastasis in multiple ipsilateral (on the same side) nodes, none larger than 6 cm in greatest dimension and ENE*(-). |
| N2c | Metastases in bilateral (on both sides) or contralateral (on the opposite side) lymph node(s), none larger than 6 cm in greatest dimension and ENE*(-). |
| N3 |
Metastasis in a lymph node larger than 6 cm in greatest dimension and ENE*(-);
or metastasis in a single ipsilateral (on the same side) node, larger than 3 cm in greatest dimension and ENE(+); or multiple ipsilateral, contralateral (on the opposite side), or bilateral (on both sides) lymph nodes, any with ENE(+); or a single contralateral node of any size and ENE(+). |
| N3a | Metastasis in a lymph node, larger than 6 cm in greatest dimension and ENE*(-). |
| N3b |
Metastasis in a single ipsilateral (on the same side) node larger than 3 cm in greatest dimension and ENE*(+);
or multiple ipsilateral, contralateral (on the opposite side), or bilateral (on both sides) nodes, any with ENE(+); or a single contralateral node of any size and ENE(+). |
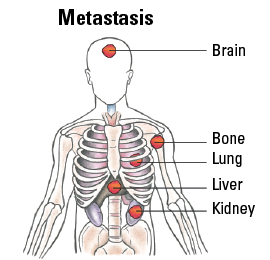
| Metastasis (M) | |
| M0 | No distant metastasis. |
| M1 | Distant metastasis. |
Staging Laryngeal Cancer
| Stage | T | N | M |
| 0 | Tis | N0 | M0 |
| I | T1 | N0 | M0 |
| II | T2 | N0 | M0 |
| III |
T3 T1, T2, T3 |
N0 N1 |
M0 M0 |
| IVA |
T4a T1, T2, T3, T4a |
N0, N1 N2 |
M0 M0 |
| IVB |
Any T T4b |
N3 Any N |
M0 M0 |
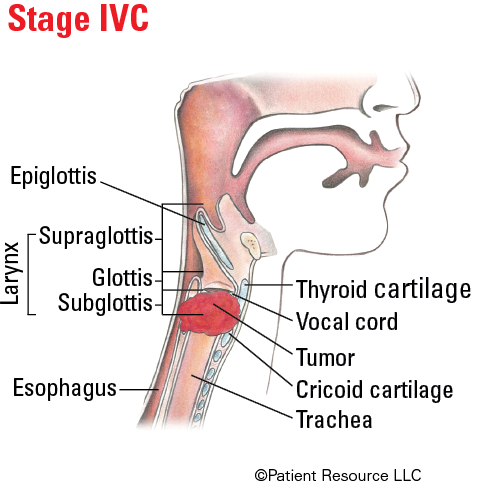
| IVC | Any T | Any N | M1 |
Illustrated Stages of Laryngeal Cancer (Supraglottis)
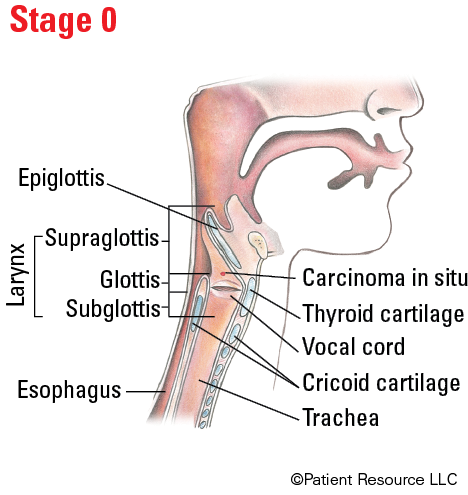
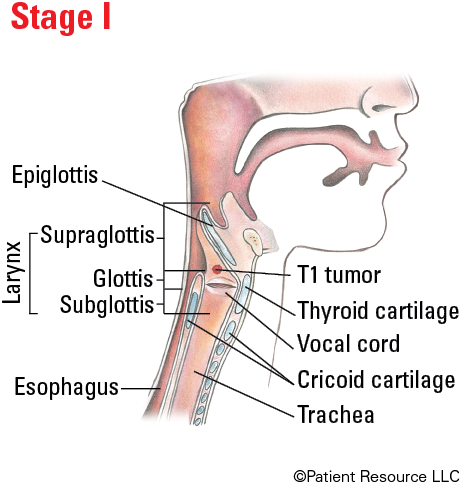
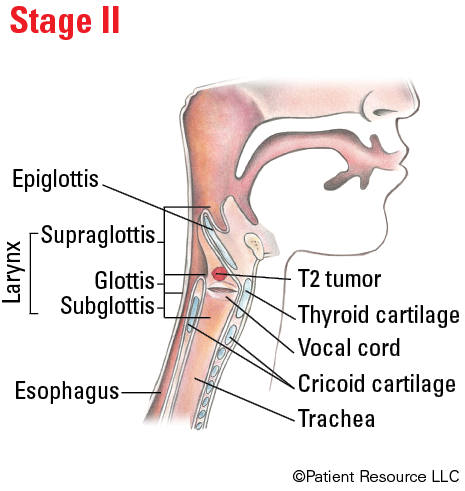
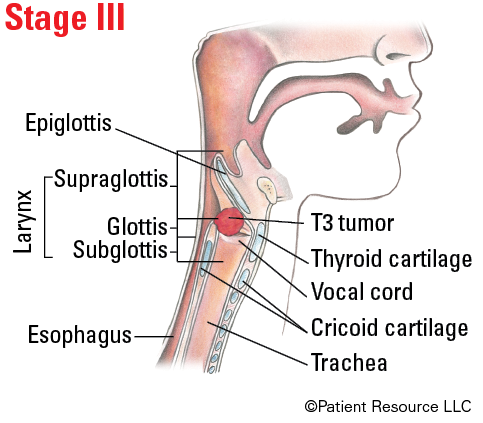
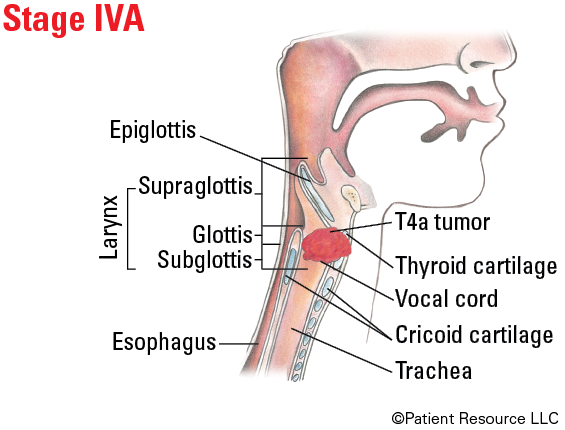
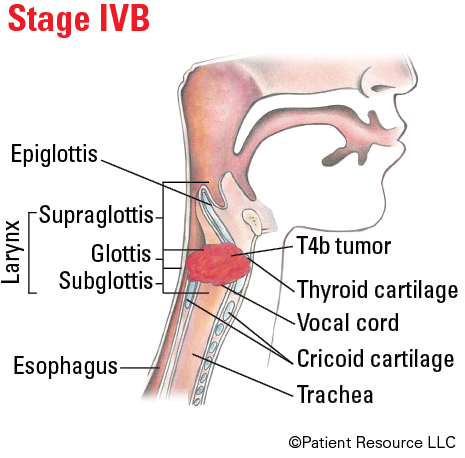
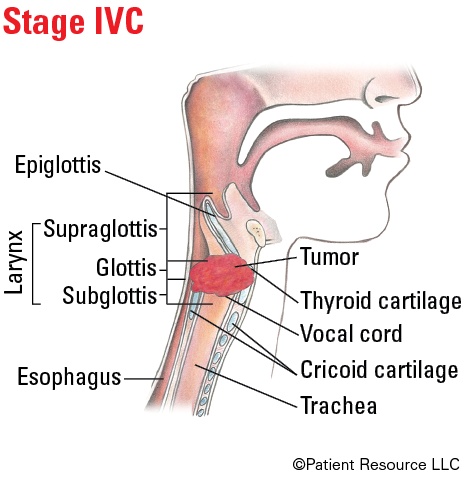
Illustrated Stages of Laryngeal Cancer (Glottis)
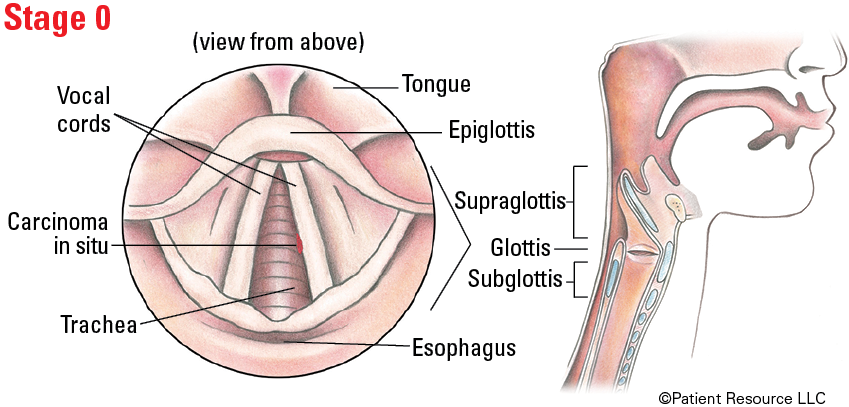
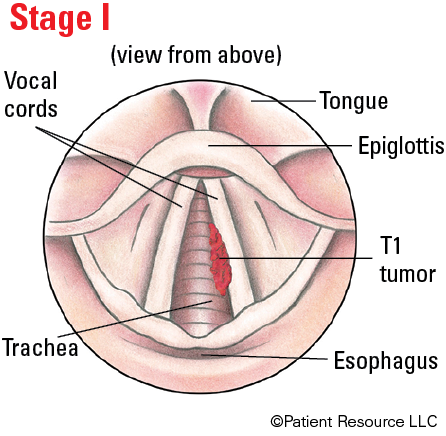
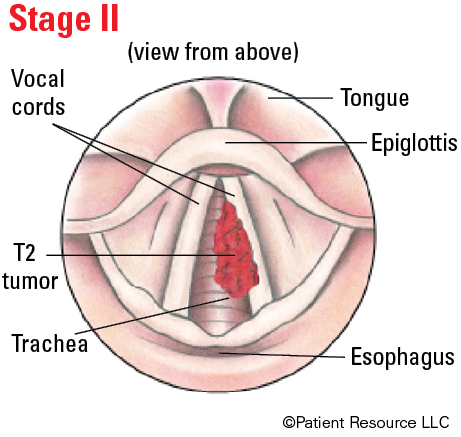
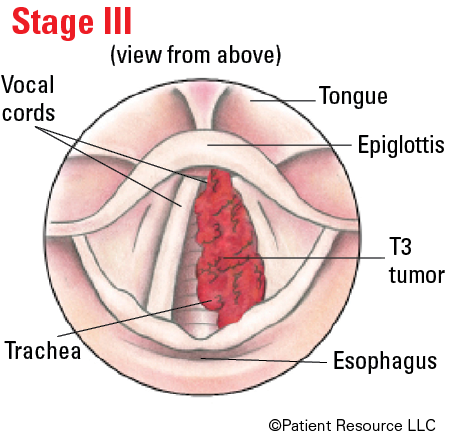
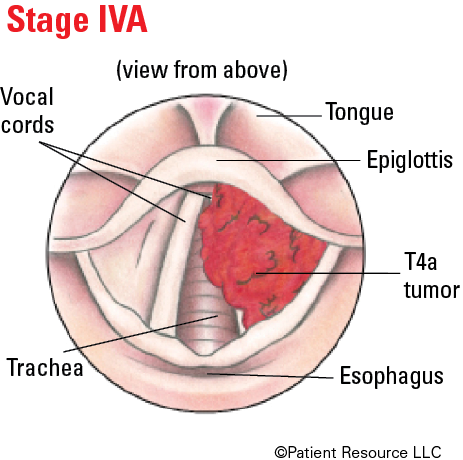
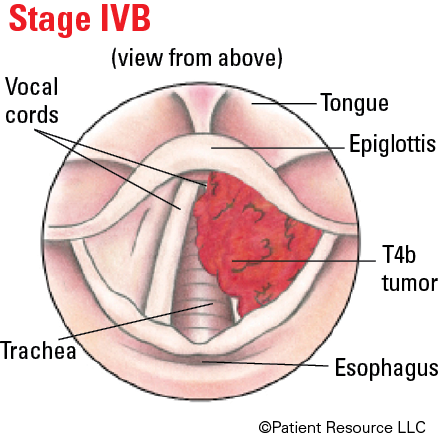
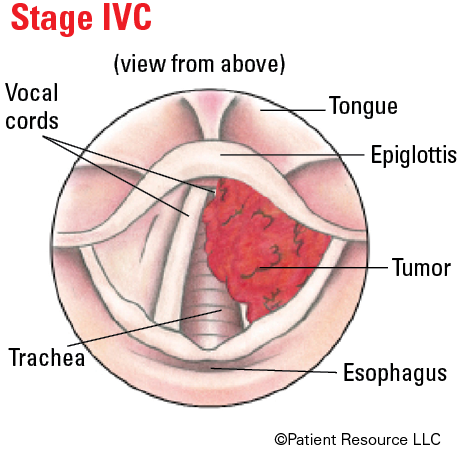
Illustrated Stages of Laryngeal Cancer (Subglottis)