Head & Neck
Throat Cancer
Includes illustrated staging details
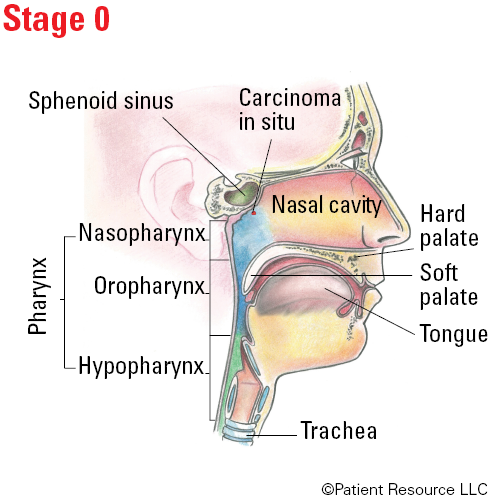
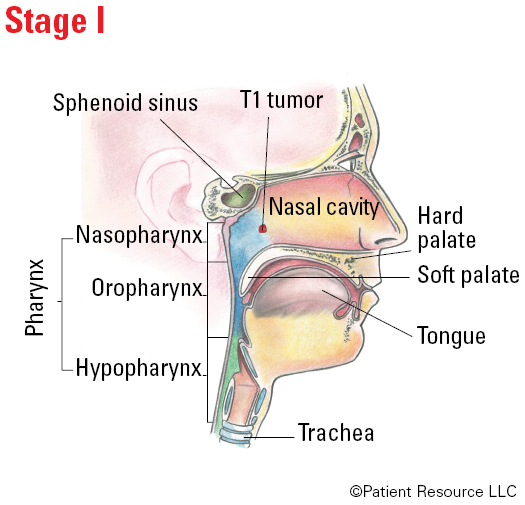
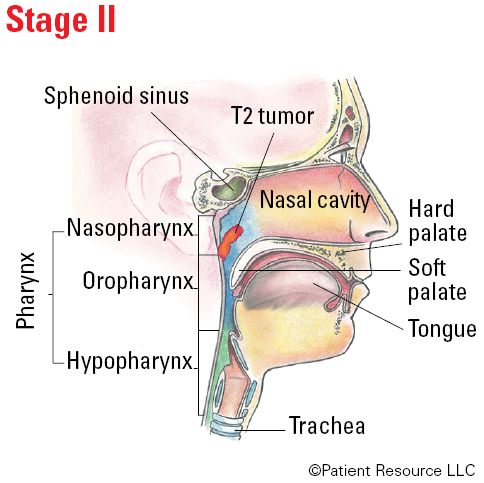
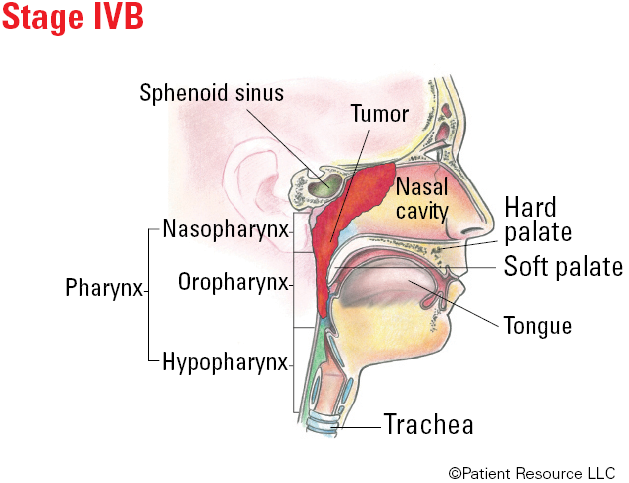
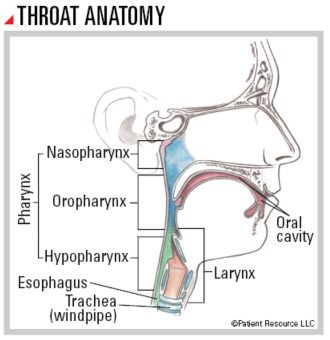
The throat, or pharynx (FAYR-inx), is a hollow tube that starts behind the nose and leads to the esophagus. As part of both the respiratory and the digestive systems, it functions as a passageway for air, food and liquid. It is divided into three parts: the nasopharynx (behind the nose); the oropharynx, which includes the soft palate (the back of the roof of the mouth), the base of the tongue and the tonsils; and the hypopharynx, which is the lowest portion of the throat. Throat cancer typically begins in the thin, flat squamous (SKWAY-mus) cells lining the mucous membranes.
The human papillomavirus (HPV) is linked to most oropharyngeal cancers. Nasopharyngeal cancer may be caused by the Epstein-Barr virus (EBV), particularly in people of Asian descent.
Treatment Options
As your doctor tailors your treatment plan, several factors will be considered during the process, including the region of the throat where the cancer occurs, whether the cancer is primary or recurrent, and the presence of certain biomarkers related to HPV. Check the staging table headlines carefully to find the ones that apply to you because different tables are used based on the HPV status and region of the throat where the cancer is located.
Throughout treatment, your doctor will try to preserve as much normal function as possible. One or more of the following options may be in your treatment plan.
Surgery is commonly used to treat oropharyngeal and hypopharyngeal cancers. It is rarely used for nasopharyngeal cancers because the area is difficult to reach. However, it may be used for nasopharyngeal cancer that does not respond to radiation therapy and to remove lymph nodes or other tissues in the neck. One or more of the following surgeries may be used.
Transoral robotic surgery (TORS) is an option for early-stage oropharyngeal cancers (especially those containing HPV+ tumors). It can be used to remove cancers from the tonsils or the back one-third of the tongue, called the base of the tongue. TORS may also be used to treat certain small hypo-pharyngeal cancers.
Radical tonsillectomy, also known as lateral oropharyngectomy, removes the tonsil as well as a cuff of tissue around the tonsil, including part of the soft palate, pharynx and base of the tongue.
Base of tongue resection removes the tumor from the back one-third of the tongue.
Partial pharyngectomy removes part of the pharynx (throat).
Laryngopharyngectomy removes tumors in the hypopharynx, the lowest part of the throat. This involves the removal of the larynx (voice box), including the vocal folds and pharynx. With this approach, a surgeon reconstructs the pharynx and creates a stoma for breathing (see Stoma Care, page 17.) This type of surgery is typically reserved for large tumors or those that fail nonsurgical treatment.
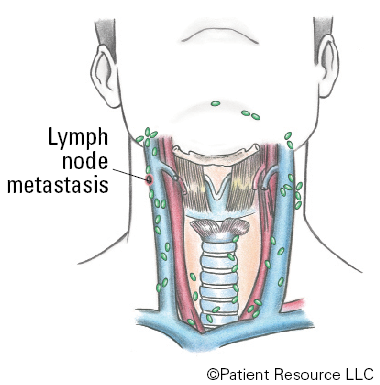
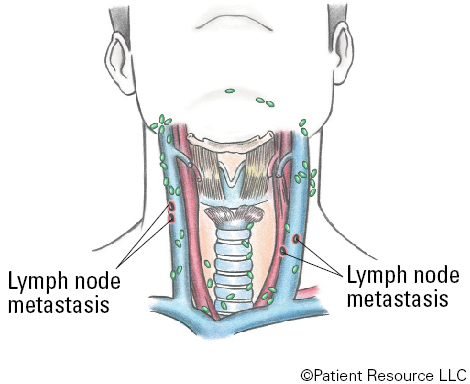
A neck dissection to remove lymph nodes may be performed.
Reconstructive surgery may be recommended to restore function or appearance and replace missing tissue. This surgery would take place at the same time the cancer is being removed (see Reconstruction & Rehabilitation).
Radiation therapy may be given alone or with chemotherapy (chemoradiation) as a first-line treatment for throat cancers in which surgery is not a good option.
External-beam radiation therapy (EBRT) is the most common type of radiation therapy used to treat throat cancers. It includes stereotactic radiation therapy, intensity-modulated radiation therapy (IMRT), and proton therapy, with IMRT being the most commonly used and well-researched.
Hyperfractionated radiation therapy, in which the radiation is given in smaller doses but more frequently, is an approach that may be used for certain cases of advanced throat cancer to improve the way the tumor responds to treatment.
Radiation with or without chemotherapy may also be recommended following surgery as adjuvant treatment for advanced stage cancers. This therapy may be used to eliminate any remaining cancer cells and to lower the risk of recurrence.
Drug therapy may be used alone or in combination with other therapies.
Chemotherapy given alone may be used to treat cancers that are not able to be removed surgically or that have returned (recurred). In this case, the goal of treatment may be to prevent growth instead of cure. It may be given after surgery with radiation therapy (chemoradiation) if the risk for recurrence is high. For nasopharyngeal cancers, additional chemotherapy may be given before starting chemoradiation treatment, also called neoadjuvant chemotherapy. Chemoradiation may be an option for the first treatment used.
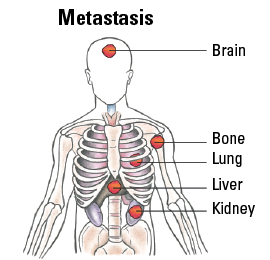
Immunotherapy in the form of immune checkpoint inhibitors may be an option for treating certain recurrent or metastatic throat cancers. The doctor will test for the tumor’s PD-L1 expression, which may indicate whether the tumor could respond to immunotherapy. If expression is more than 1 percent, the tumor is considered to be PD-L1 positive and immunotherapy alone may be used. If PD-L1 is negative, immunotherapy and traditional chemotherapy are often combined for patients who have recurrent or metastatic cancer. It may also be used if the cancer continues to grow or spread during treatment with platinum-based chemotherapy.
Targeted therapy drugs may treat types of throat cancer that contain specific genetic abnormalities, proteins or growth factors. Epidermal growth factor receptor (EFGR) inhibitors are approved for oropharyngeal and hypopharyngeal cancers in combination with radiation therapy or chemotherapy.
TNM Classification for Oropharyngeal (HPV-) and Hypopharyngeal Cancers
| Classification | Definition |
| Tumor (T) | |
| TX | Primary tumor cannot be assessed. |
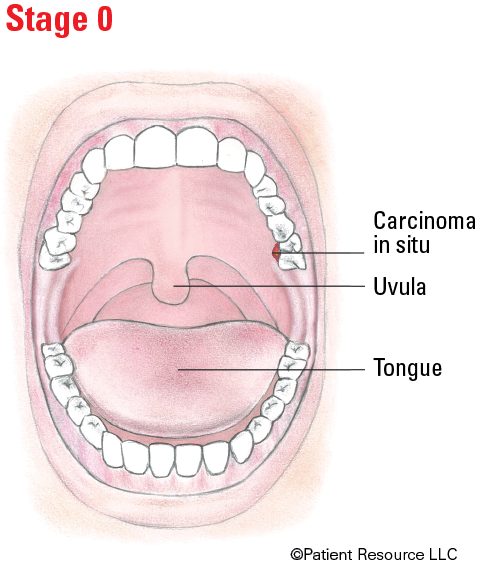
| Tis | Carcinoma in situ. |
| >Oropharyngeal (HPV-) | |
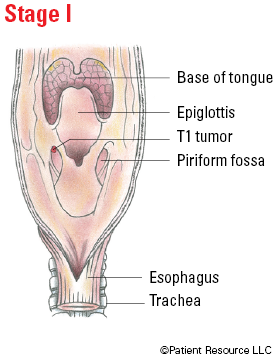
| T1 | Tumor 2 cm or smaller in greatest dimension. |
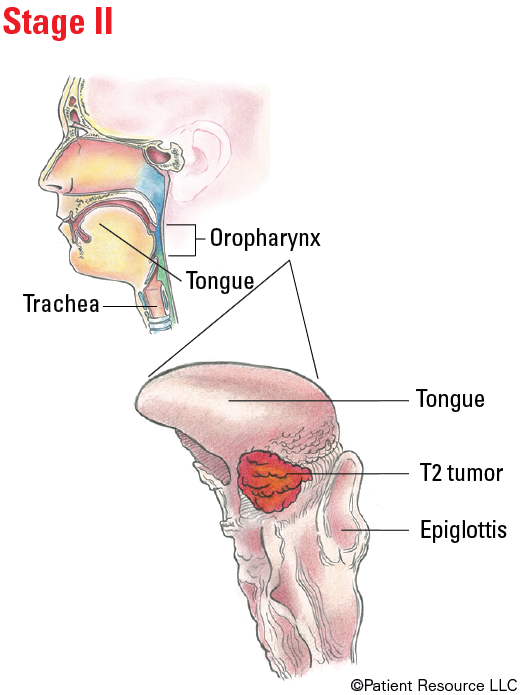
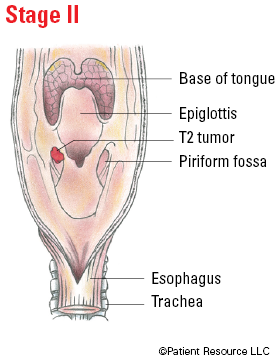
| T2 | Tumor larger than 2 cm but not larger than 4 cm in greatest dimension. |
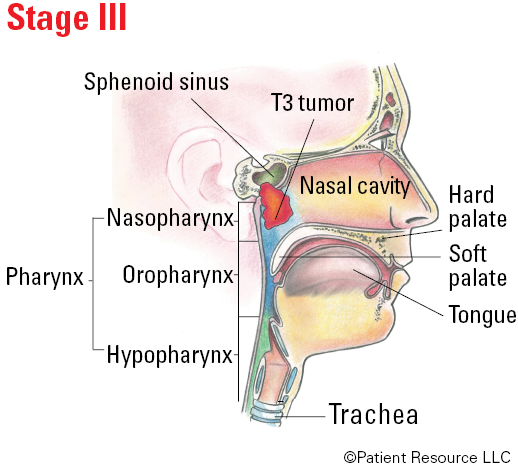
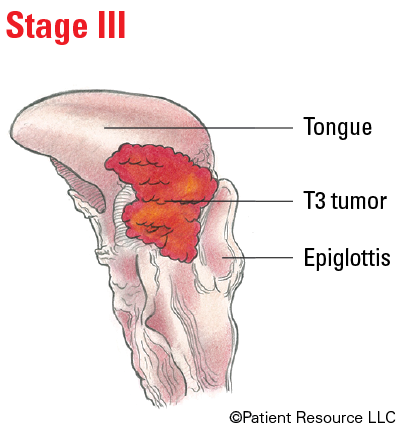
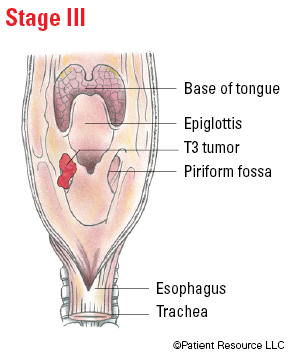
| T3 | Tumor larger than 4 cm in greatest dimension or extension to lingual surface of epiglottis. |
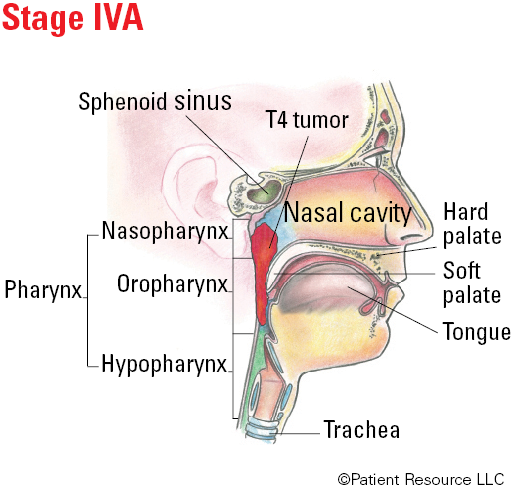
| T4 | Moderately advanced or very advanced local disease. |
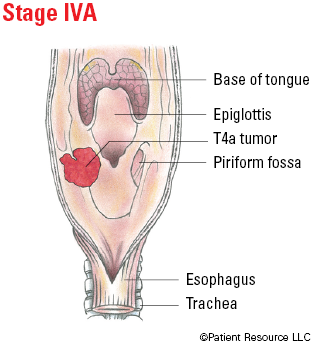
| T4a | Moderately advanced local disease. Tumor invades the larynx, extrinsic muscle of tongue, medial pterygoid, hard palate or mandible (jawbone). |
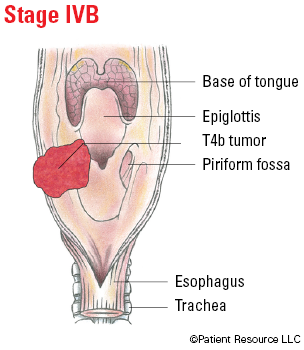
| T4b | Very advanced local disease. Tumor invades lateral pterygoid muscle, pterygoid plates, lateral nasopharynx, or skull base or encases carotid artery. |
| Hypopharyngeal | |
| T1 | Tumor limited to one subsite of hypopharynx and/or 2 cm or smaller in greatest dimension. |
| T2 | Tumor invades more than one subsite of hypopharynx or an adjacent site, or measures larger than 2 cm but not larger than 4 cm in greatest dimension without fixation of hemilarynx. |
| T3 | Tumor larger than 4 cm in greatest dimension or with fixation of hemilarynx or extension to esophageal mucosa. |
| T4 | Moderately advanced and very advanced local disease. |
| T4a | Moderately advanced local disease. Tumor invades thyroid/cricoid cartilage, hyoid bone, thyroid gland, esophageal muscle or central compartment soft tissue. |
| T4b | Very advanced local disease. Tumor invades prevertebral fascia, encases carotid artery or involves mediastinal structures. |
| Node (N) | |
| NX | Regional lymph nodes cannot be assessed. |
| N0 | No regional lymph node metastasis. |
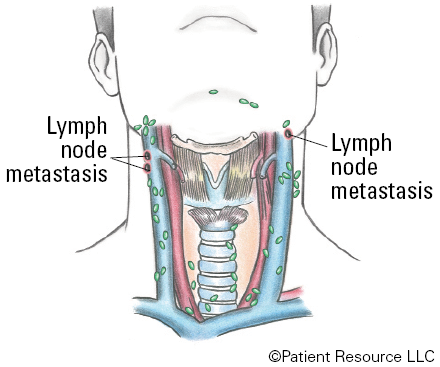
| N1 | Metastasis in a single ipsilateral (on the same side) lymph node 3 cm or smaller in greatest dimension and ENE*(-). |
| N2 |
Metastasis in a single ipsilateral (on the same side) lymph node 3 cm or smaller in greatest dimension and ENE*(+);
or larger than 3 cm but not larger than 6 cm in greatest dimension and ENE(-); or metastases in multiple ipsilateral lymph nodes, none larger than 6 cm in greatest dimension and ENE(-); or in bilateral (on both sides) or contralateral (on the opposite side) lymph node(s), none larger than 6 cm in greatest dimension and ENE(-). |
| N2a |
Metastasis in single ipsilateral (on the same side) node 3 cm or smaller in greatest dimension and ENE*(+);
or a single ipsilateral node larger than 3 cm but not larger than 6 cm in greatest dimension and ENE(-). |
| N2b | Metastasis in multiple ipsilateral (on the same side) nodes none larger than 6 cm in greatest dimension and ENE*(-). |
| N2c | Metastasis in bilateral (on both sides) or contralateral (on the opposite side) lymph node(s), none larger than 6 cm in greatest dimension and ENE*(-). |
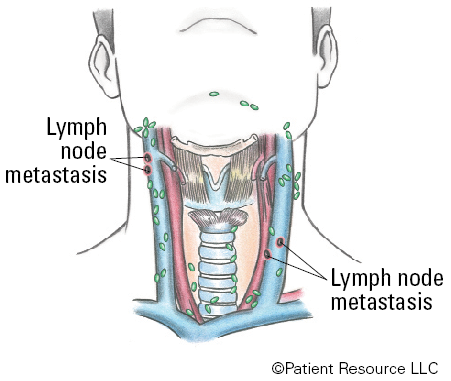
| N3 |
Metastasis in a lymph node larger than 6 cm in greatest dimension and ENE*(-);
or metastasis in a single ipsilateral (on the same side) node larger than 3 cm in greatest dimension and ENE*(+); or multiple ipsilateral, contralateral (on the opposite side) or bilateral (on both sides) nodes, any with ENE(+); or a single contralateral node of any size and ENE(+). |
| N3a | Metastasis in a lymph node larger than 6 cm in greatest dimension and ENE*(-). |
| N3b |
Metastasis in a single ipsilateral (on the same side) node larger than 3 cm in greatest dimension and ENE*(+);
or multiple ipsilateral, contralateral (on the opposite side) or bilateral (on both sides) nodes, any with ENE(+); or a single contralateral node of any size and ENE(+). |
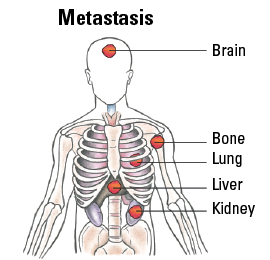
| Metastasis (M) | |
| M0 | No distant metastasis. |
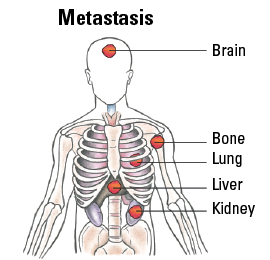
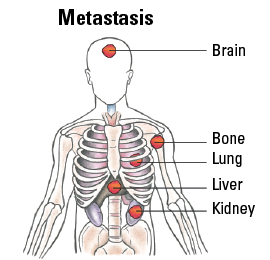
| M1 | Distant metastasis. |
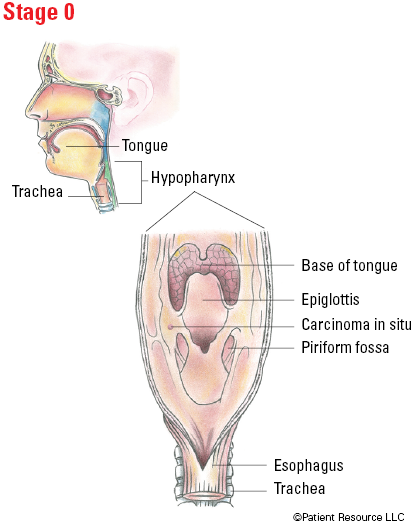
Staging Oropharyngeal (HPV-) and Hypopharyngeal Cancers
| Stage | T | N | M |
| 0 | Tis | N0 | M0 |
| I | T1 | N0 | M0 |
| II | T2 | N0 | M0 |
| III |
T3 T1, T2, T3 |
N0 N1 |
M0 M0 |
| IVA |
T4a T1, T2, T3, T4a |
N0, N1 N2 |
M0 M0 |
| IVB |
Any T T4b |
N3 Any N |
M0 M0 |
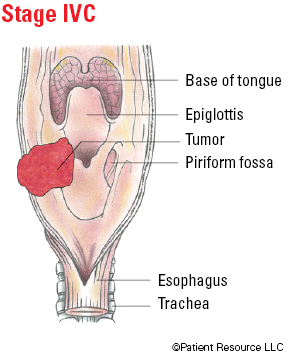
| IVC | Any T | Any N | M1 |
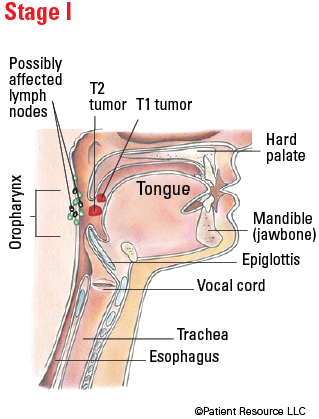
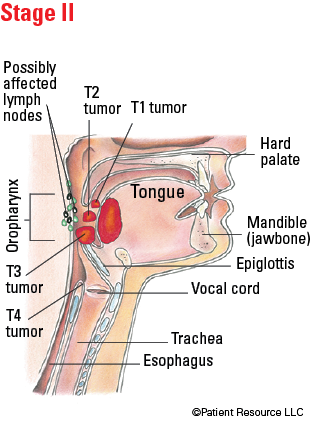
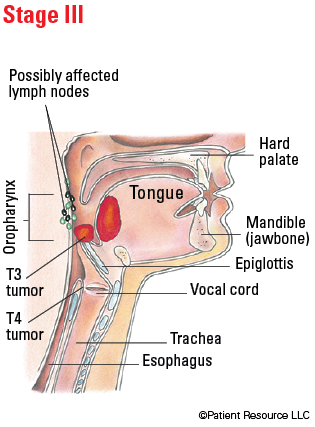
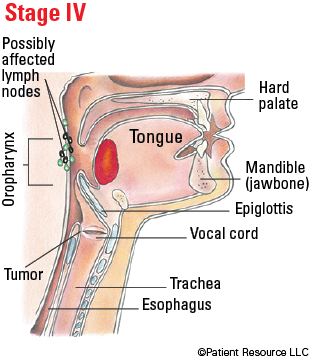
Illustrated Stages of Oropharyngeal (HPV-) Cancer

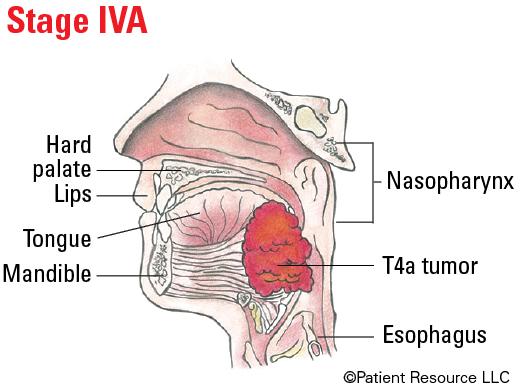
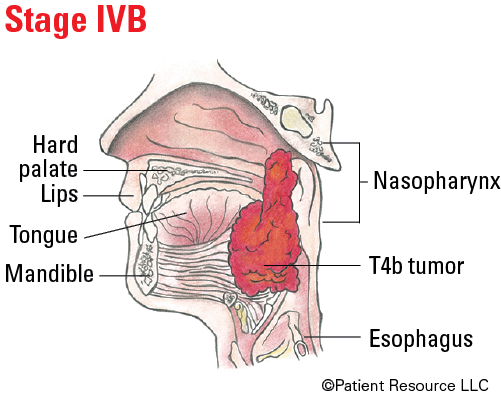
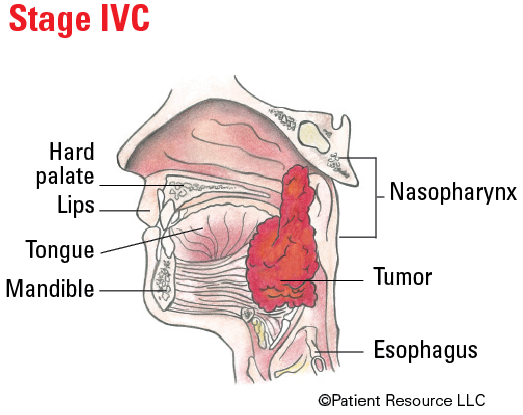
Illustrated Stages of Hypopharyngeal Cancer
Classifying & Staging Oropharyngeal (HPV+) Cancer
| Classification | Definition |
| Tumor (T) | |
| T0 | No primary identified. |
| T1 | Tumor 2 cm or smaller in greatest dimension. |
| T2 | Tumor larger than 2 cm but not larger than 4 cm in greatest dimension. |
| T3 | Tumor larger than 4 cm in greatest dimension or extension to lingual surface of epiglottis. |
| T4 | Moderately advanced local disease. Tumor invades the larynx, extrinsic muscle of tongue, medial pterygoid, hard palate or mandible (jawbone) or beyond. |
| Node (N) | |
| NX | Regional lymph nodes cannot be assessed. |
| N0 | No regional lymph node metastasis. |
| N1 | Metastasis in four or fewer lymph nodes. |
| N2 | Metastasis in more than four lymph nodes. |
| Metastasis (M) | |
| M0 | No distant metastasis. |
| M1 | Distant metastasis. |
| Stage | T | N | M |
| I | T0, T1, T2 | N0, N1 | M0 |
| II |
T0, T1, T2
T3, T4 |
N2
N0, N1 |
M0
M0 |
| III | T3, T4 | N2 | M0 |
| IV | Any T | Any N | M1 |
Illustrated Stages of Oropharyngeal (HPV+) Cancer
Classifying & Staging Nasopharyngeal Cancer
| Classification | Definition |
| Tumor (T) | |
| TX | Primary tumor cannot be assessed. |
| T0 | No tumor identified, but EBV-positive cervical node(s) involvement. |
| Tis | Carcinoma in situ. |
| T1 | Tumor confined to nasopharynx (behind nasal cavity/upper part of throat), or extension to oropharynx and/or nasal cavity without parapharyngeal involvement. |
| T2 | Tumor with extension to parapharyngeal space, and/or adjacent soft tissue involvement (medial pterygoid, lateral pterygoid, prevertebral muscles). |
| T3 | Tumor with infiltration of bony structures at skull base, cervical vertebra, pterygoid structures, and/or paranasal sinuses. |
| T4 | Tumor with intracranial extension, involvement of cranial nerves, hypopharynx, orbit, parotid gland, and/or extensive soft tissue infiltration beyond the lateral surface of the lateral pterygoid muscle. |
| Node (N) | |
| NX | Regional lymph nodes cannot be assessed. |
| N0 | No regional lymph node metastasis. |
| N1 | Unilateral (on one side) metastasis in cervical lymph node(s) and/or unilateral or bilateral metastasis (on both sides) in retropharyngeal lymph node(s), 6 cm or smaller in greatest dimension, above the caudal border of cricoid cartilage. |
| N2 | Bilateral metastasis in cervical lymph node(s), 6 cm or smaller in greatest dimension, above the caudal border of cricoid cartilage. |
| N3 | Unilateral (on one side) or bilateral (on both sides) metastasis in cervical lymph node(s), larger than 6 cm in greatest dimension, and/or extension below the caudal border of cricoid cartilage. |
| Metastasis (M) | |
| M0 | No distant metastasis. |
| M1 | Distant metastasis. |
| Stage | T | N | M |
| 0 | Tis | N0 | M0 |
| I | T1 | N0 | M0 |
| II |
T0, T1, T2
T2 |
N1
N0 |
M0
M0 |
| III |
T0, T1, T2, T3
T3 T3 |
N2
N0 N1 |
M0
M0 M0 |
| IVA |
T4
T4 T4 Any T |
N0
N1 N2 N3 |
M0
M0 M0 M0 |
| IVB | Any T | Any N | M1 |
Illustrated Stages of Nasopharyngeal Cancer